Bronchitis
 Acute Bronchitis
Acute Bronchitis
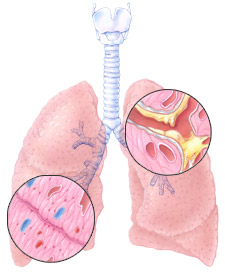
Bronchitis is an inflammation (thickening and/or swelling) of the lining of the bronchi and increased mucus production. Inflammation can be caused by: smoke, infections, chemicals, pollution, and/or acids from your stomach (gastroesophageal reflux disease, GERD).
Many people have had a brief attack of bronchitis, often after you have had a cold. The attack usually lasts for about a week, but the cough may last up to three weeks. During a bout with bronchitis, you may experience cough with large amounts of mucus production, and sometimes, a fever.
This brief type of bronchitis is called Acute Bronchitis—each attack does not last long and does not come back again and again. Lung function returns to normal after the bronchitis infection has ended.
Acute bronchitis is not COPD.
Image © peggerrity.com
Chronic Bronchitis
Chronic bronchitis is an ongoing illness that can cause serious long-lasting lung problems. The signs and symptoms of chronic bronchitis are:
- A cough with mucus production that lasts at least for three months
- The productive cough is present for two years in a row
Of course other diseases must be excluded before chronic bronchitis can be diagnosed (see insert).
Chronic Bronchitis
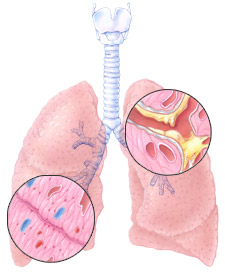
Chronic bronchitis is a condition when repeated lung inflammation damages the lungs. Chronic inflammation in the lungs causes scarring of the airways and excessive production of mucus that results in a chronic cough. Some call it a “smoker’s” cough.
As the lining of the airways becomes thickened and narrow/obstructed (due to the scarring) less air is moved in and out of the lungs. Air becomes trapped in the lungs and this limits the amount of air that you are able to breathe in with each breath.
If the inflammation continues and the cough becomes more regular (a daily event rather than just periods of coughing) this can progress to the point where shortness of breath is present. Chronic bronchitis can exist alone, before, or during emphysema.
COPD has no cure, yet there are treatments (see Treatment), along with the removal of irritants that will decrease the effects of COPD.
Image © peggerrity.com
Emphysema
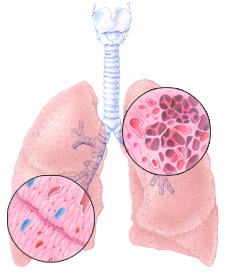 Emphysema develops when many of the small air sacs or alveoli in the lungs get stretched out and lose their ability to empty out all of the air. Air becomes trapped in the alveoli and the alveoli become stretched out and over-inflated.
Emphysema develops when many of the small air sacs or alveoli in the lungs get stretched out and lose their ability to empty out all of the air. Air becomes trapped in the alveoli and the alveoli become stretched out and over-inflated.
This damage can cause the alveoli to come apart (rupture), and form one large air space instead of many small ones. The destruction of healthy air sacs makes it difficult for the lung to work properly.
There are less alveoli to deliver oxygen to the bloodstream. The damage is progressive and, as lung tissue does not repair itself, the damage is permanent. The whole body suffers when the lung cannot deliver the essential oxygen and remove the carbon dioxide waste.
Image © peggerrity.com
Emphysema
The increased pressure of the trapped air, over time, will shorten and flatten the diaphragm. This change in the shape of the diaphragm makes it much harder for the diaphragm to play its part in moving air in and out of the lungs. The diaphragm muscle becomes weak and fatigued.
An additional result of the trapped air is that the chest cavity becomes larger (barrel chest) and the muscles in between the ribs become stretched out.
The change in the muscles of breathing significantly increase the work of breathing. Normally, the muscles of breathing require a low level of oxygen at rest (1 to 3%) but when you have COPD, the needed oxygen increases to as high as 25%.
COPD has no cure, yet there are treatments (see Treatment), along with the removal of irritants that will decrease the effects of COPD.