|
||||||||

Archive: Dr. Tom 55 Coughed up Blood and have Questions about Chest X-Ray Now four years after I coughed up a bit of blood and went to see my doctor and asked for chest x-ray. Results came back that my lungs are bigger and there is some shading in LLL. Can this be scarring or something more serious? By the way, I am smoker and have just quit after this. Bob A. Dear Bob, Better follow up on this. With a smoking history and a chest shadow, there is always the fear of lung cancer. Check with you pulmonologist or get a referral. Dr. Tom
Needs Answer about Lung Nodules They sent me for a PET Scan (Positron Emission Tomography – a test often used to detect cancer) and saw the nodule but no hot spots (malignancies light up as “hot spots” in the image). Follow-up 12-17-05 Impression: 1. Right middle lobe essentially unchanged when compared to 09-14-05 right hilar adenopathy. 2. Shotty left hilar nodes. 3. New patchy linear changes related to the lingual. I don’t know what all this means. My doctor has never sat with me and explained what’s going on. Not that I haven’t tired. I had to go for another CT Scan this month on 03-06-06. When should I see a specialist? Where do I start? Should I be worried? Please help. Melissa A. Dear Melissa, I suggest seeing a pulmonologist now. These findings need explanation. Dr. Tom
Aches and Pains Now Affecting His Home Life Now my main problem is my right throat has been irritated for the last 10 years. I took antibiotics several times, but no use. I have pain in somewhere in airway to the right lung when I take a deep breath. Feel like mucus membrane is damaged (dry feeling) in my lower right throat. I have recurrent pain in between my right shoulder blade and the spine. Two years back I did sinus and thorax CT scan and all normal except mucus thickening in maxillary sinus. Recently I had a 45-degree endoscope and doctor prescribed medicines for acid reflux but I don’t think that is my main problem. I never had a bronchoscope. My other symptoms are fatigue, pain in my shoulders, numbness on my palm, elevated BP, palpitation, headache, unexplained back pain, dry eyes, blocked right nose, dry cough recently started. etc. No one could diagnose my exact problem. Now it’s affecting my family life because I am always thinking about my condition and gloomy. Any advice highly appreciated. Nibi A. Dear Nibi, You have a lot of symptoms that need a diagnosis. I suggest seeing a specialist, such as a pulmonologist, or allergist. Dr. Tom
Questions about Sarcoidosis Also I’ve been having chest pain and SOB but he said that there is no physiological reason for it by looking at my HRCT (High Resolution CT Scan) and suggests that it is anxiety; although I highly dispute that assessment because it occurs at rest and under no anxiety inducing situations. Having mild ILD without adenopathy couldn’t cause chest pain and SOB? Jeremy A. Dear Jeremy, The chest pain is probably not from sarcoidosis. You need spirometry (a test to measure lung function that can be done in a doctor’s office. See: National Lung Health Program NLHP https://www.nlhep.org/spirom1.html ). If abnormal, this may explain your shortness of breath. HRCT does NOT test lung function! Dr. Tom
How Can You Determine how Severity of Interstitial Pneumonitis? I went on Prednisone, which eliminated all of the coughing, shortness of breath, and low blood oxygen level. I went on the slow tapering off program. I was off the Prednisone for about a month, and then I started coughing again. I am going to try a small dose to curb that if I can. I would like to know if it is a good idea to have another CT Scan to see how much it has progressed. I was told a lung biopsy is the only way to tell how far it has progressed. My fear is that there is inflammation in there now that I should be treating. What is your opinion? Betty A. Dear Betty, You should start with lung function testing, by spirometry (a test to measure lung function that can be done in a doctor’s office. See: National Lung Health Program NLHEP https://www.nlhep.org/spirom1.html ) to see about your airflow and air volume. A diffusion test (used to determine how well oxygen passes from the air sacs of the lungs into the blood) is often useful in interstitial pneumonitis. See a pulmonologist. You should strive to maintain lung function, and if steroids are effective, they should be continued under the direction of your doctor. Dr. Tom
Need Respiratory Therapy Duties for School Project Shawn A. Dear Shawn, Consult the American Association for Respiratory Care’s website for information on careers in respiratory care. They have a wealth of information about this interesting profession. Dr. Tom
Just Diagnosed with Severe Emphysema Can I do active exercise? Will I have to have treatment? A specialist who is doing an examination found emphysema but told me nothing about how it is treated. I am a bit scared of the future. Pauline A. Dear Pauline, Did this “specialist” do lung function testing, i.e. simple spirometry? The chest x-ray is not a lung function test. Your doctor should know this. Maybe you need to change doctors. Dr. Tom
Worried about Mom Sir please help and advice some better treatment, she is only 50 years old. Sonal A. Dear Sonal, This is not my area of expertise. I suggest you consult a rheumatologist. He will know about the most appropriate treatment for osteoporosis and psoriasis. Dr. Tom
Strange Fibers and Particles in Home The contents were analyzed as cellulose 60%. I have constant sinus infections, and ear problems. My husband coughs and it sounds like a dog barking. Lately, we both have had problems with vertigo and dizziness. My daughter gets severe headaches when she visits too long, plus last week she had vertigo and had to miss work for a night. We also have water under our home and smell a dirt smell in our bathrooms. We clean sometimes two times a day to keep the dust and dirt down. I am terrified due to breathing in these particles. Any suggestions? Ruth A. Dear Ruth, You may have mold under your house that is causing these symptoms. I can’t imagine why you have so much dust. Is there a defect in your house? Dr. Tom
Is There a High Flow Oxygen System for Home Use Rudy A. Dear Rudy, There is one high flow concentrator on the market. I can’t remember its name. Consult your oxygen supplier. This is a very high flow rate, and not achievable by conventional systems. Check with Transtracheal systems of Denver, i.e. [email protected]. They know about high flow systems. Dr. Tom
What is a Low Reading on and Oximeter? Pat A. Dear Pat, Normal oxygen saturation at sea level is 94-97%. In Denver it is 92-94% because of the altitude. Lower at higher levels such as Leadville, CO, elevation 10K feet, where normal is 85%. In general low levels are below 90% at most usual locations. Dr. Tom
Two Different Opinions on Results of Mother’s Scans After three months she went for her second follow-up. Chest x-rays showed both her lungs filled with “junk”. She was told she might have gotten a cold and needed to bring up the phlegm. Her pulmonary doctor put her on steroids. Four days later there was no change in x-rays...now my mom is short of breath and coughing up clear phlegm. The doctor scheduled her for a brochoscopy...have not received results yet but pulmonary doctor thinks it might be a tumor? How could this be? We were told she was practically cancer free. She was even nominated to model for a fund raiser on behalf of cancer survivors! Could this be some kind of disease or bacteria? Could the cancer come back and invade both lungs in just three months? Both the surgeon and her oncologist do not think it is cancer but her pulmonary does...Very confused and frustrated ...would appreciate any advice you can give. Monica A. Dear Monica, I doubt if it is cancer, in such a short time. You need a diagnosis from your pulmonologist. He may well do a bronchoscopy (a diagnostic procedure in which your doctor uses a scope, a tube with a camera on the end, to take a look at the inside of the airways and lungs). Dr. Tom
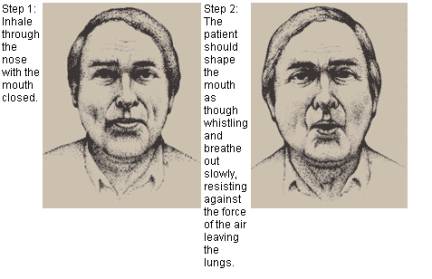
Any Treatment for Hyperventilation Syndrome Eventually, my primary care doctor diagnosed me with possible hyperventilation syndrome. I do not have panic attacks, etc., but rather, my ‘over breathing’ is very subtle. I’ve been told that even subtle changes in breathing patterns can upset my oxygen/C02 (oxygen/carbon dioxide) balance, which can produce strange symptoms. My question is: Are there any exercises that I can do to “re-set” my breathing? My GP was at a loss as to this question; he said that there were no exercises that he knew of, because consciously thinking about your breathing can make the problem worse. Are there really no exercises or treatment for hyperventilation syndrome? Should I try to see a respiratory therapist? Thanks in advance for your feedback. Mia A. Dear Mia, Shortness of breath from hyperventilation usually is relieved by any exercise, such as walking. Practicing slow breathing with exhalation against pursed lips, as in whistling may help. You will probably get over these symptoms.
Dr. Tom
Coughing for Three Months I have been to the hospital and been given chest x-rays that were clear. They have said things from maybe allergies and I was given Zyrtec 10 mg. The Zyrtec didn’t work. I was told another time maybe I had bronchitis. I went back to the hospital and took some of the stuff to show them. They said they couldn’t believe I spit it up. They made me feel as if I was crazy. I think they didn’t know what in the world I had been spitting up. They said they would do a test on it to see if it contained a bacteria and they would let me know if it did. They said I needed to be seen by a pulmonologist. I don’t have any insurance and will not be able to see one for a while. I was wondering if maybe you could shed some light on what may be happening to me. I have been in pretty good health. I have not had any pain and I am not running any fever. I have been getting around-100 percent oxygen. I do smoke though. I am working on quitting now. Kimberly A. Dear Kimberly, This is most likely heavy mucus from smoking. Key to getting better is stopping all smoking. I realize this is difficult, but you have to do it. Cold turkey method is best. Nicotine gum may help. If this continues you need to see a pulmonologist even if you do not have insurance. You will have a lot more money when you finally stop smoking. Good luck. Dr. Tom
Asthma Medication Question Now for the last two weeks I am giving montelukast ( also known as Singular, it is a control or maintenance drug for the treatment of asthma) 5 mg. daily in the evening, she shows some relief. Now. I am worried about the side effects of steroids, as it may be the cause of stunted growth, reduced immunity etc. I also wanted to know the side effect of long-term use of montelukast sodium. Which medication will be good for her? Both the parents have history of asthma. Please reply me. Hasi A. Dear Hasi, This asthma has to be controlled, not matter what drug it takes. Uncontrolled asthma will stunt growth. Inhaled steroids will not have much if any effect on growth, and growth will be encouraged by controlling the asthma. Montelukast is a safe drug, but I do not know about long term side effects, particularly in children. I am sure that controlling the asthma is the top priority. Dr. Tom
Chewing Tobacco and COPD TJ A. Dear TJ, No, but it will often cause severe problems in your mouth. Better stop this too. DR Tom
Mother had Another Chest X-Ray What is the chance of this being pneumonia? Or does this sound like cancer to you? She is feeling much better and she’s not spitting up blood or passing any. I know that is one of the signs of lung cancer. Jennifer A. Dear Jennifer, Pneumonia may take weeks to clear. You need a follow up in three months to see if the shadows have resolved. If not, your mom needs further investigation. Dr. Tom Click here to read Jennifer’s previous question... Can Spot Seen on Chest X-Ray be Pneumonia? They have given her an antibiotic in case the spots are from pneumonia. They said the spots would be gone in seven days if it was pneumonia so in seven days, from the first day, they will do another chest x-ray to see if the spots are still there. What else could this be? She has been having to sleep sitting up due to the pain in her chest, but taking the antibiotic she says her chest isn’t hurting with every breath anymore. Do you think the spots are caused by something that the antibiotic is going to take care of? Jennifer A. Dear Jennifer, The spots need to be followed closely. They could be a variety of things, both benign and malignant. If there is a growing spot or mass, it needs to be biopsied. Dr. Tom
Warfarin and Severe COPD Bill RN A. Dear Bill, This is hard to explain, but you cannot argue with success. I do not know the reason why the warfarin was started in the first place. It conceivably could be for pulmonary clots, and if so, this may be the explanation. Good question! Dr. Tom
Questions about Pediatric Ventilators and Asks for a Source for Employment here in the USA Also we are closing (the military base) as you know, and I have a soldier here that is interested in coming up there for the sleep lab, he is certified in that and is a CRT. He is wanting to come up there and talked to a SGT Gray. Do you know who he is to talk to up there? I really appreciate that time and the help you give us. SGT. Collin A. Dear SGT. Collin, I found the following reference in my file that may be useful: Dockery DW, Berkey CS, Ware JH, Speizer FE, Ferris BG: Distribution of forced vital capacity and forced expiratory volume in one second in children 6 to 11 years of age. Am Rev Respir Dis 128:725-734, 1983. I hope this helps. Dr. Tom |
||
| 2025 American Association for Respiratory Care | ||