|
||||||||

Archive: Dr. Tom 52 Severe Chronic Cough Sheila A. Dear Sheila, Better get an answer from a pulmonologist. Start with a chest x-ray and spirometry to test your pulmonary function (the health of your lungs). There are many possibilities, including chronic bronchitis, lung cancer, and on and on. I cannot tell from what you tell me. Dr. Tom
What Effect do Allergies have on Breathing? I have emphysema and asthma. No chronic bronchitis. I rarely cough. Anyway, I have a skin condition that itches and my doctor, prescribed me Hydroxyzine HCL (antihistamine), 10mg, along with some creams, to help relieve the itch. What it did was clear up my allergies. I have suffered horrific allergies since 1991. In doing so, my ability to breath has improved almost 100%. Some days I wake up and forget to use my inhalers, I feel that good. I do use them, as it wouldn't be very smart otherwise. I use my nebulizer much less now. I can walk up-hill with little or no SOB (shortness of breath). My question, can clearing up allergies improve one's breathing? I've been feeling good for almost 1 1/2 months now. Thank you very much for your help. . Pat A. Dear Pat, Yes, allergies can be involved in asthma. Avoiding allergens can help. Dr. Tom
Concerned about Mum’s Chest X-Ray Mum is a life long non smoker, her husband and kids don't smoke either. Her parents smoked but she stopped living with them 40 years ago. She doesn't wheeze or cough or get bronchitis. We are very concerned - what could have caused the hyperinflation or COPD? Kris A. Dear Kris, Hyperinflation on a chest x-ray, just indicates that the patient can take a big breath. It does not measure lung function and by itself, does not mean much. If the nodule is calcified, it is indeed a granuloma. If not, it needs follow-up. Lung cancer is not common in non smokers, but does occur, particularly in women. Dr. Tom
Best Location for Someone who has Severe Emphysema Joyce A. Dear Joyce, There is no ideal climate. In general a warm, dry climate is preferred by many, and at a low altitude. Examples are New Mexico, Texas and Arizona, but not in the mountains. Dr. Tom
Registered Respiratory Therapist has a Few Questions
Gerry A. Dear Gerry, The extra one liter at sleep is empirical, not based on good science. Hypoxemia (low levels of oxygen in the blood) is usually worse during sleep due to the mismatching of ventilation and perfusion and reduced respiratory center activity. Rhinorrhea may be due to nasal irritation from the oxygen flow. Rhinorrhea, is not a symptom of interstitial fibrosis. Dr. Tom
Awakens from Sleep Starved for Air However, I have a general question, I have a problem with sleep where I stop breathing and due to this I get a shock throughout my body that wakes me up starving for air. This happens every night and shortly after going to sleep (10-20 minutes into sleep) so I can only assume that sleep apnea is not the cause, as all literature I've ever read states that sleep apnea occurs in REM sleep (Rapid Eye Movement sleep is associated with dreaming and paralysis of body muscles, except for the eye and diaphragm muscles), and I do not snore. What are other possibilities for the cause? Could sarcoidosis granulomas inflammation in the tonsils or larynx or somewhere else in that area cause this to happen? Jeremy A. Dear Jeremy, Sleep apnea can occur at any time, but usually during REM sleep. You could have some upper airway obstruction from sarcoidosis that is causing your problem. I suggest a formal sleep apnea study. Dr. Tom
Question about Granulomas Robin A. Dear Robin, Asthma and granulomas are not related. Pleural inflammation may leave a scar. Dr. Tom
Effect of High Concentration of Oxygen on COPD Patients Aida A. Dear Aida, Probably not much, but there is no point in giving more oxygen than needed. Dr. Tom
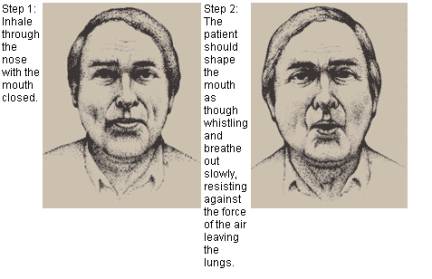
Teaching Pursed Lip Breathing during Exercise I have been able to get quite a bit of information off the Internet and different websites but one thing I am having problems understanding is purse lip breathing with exercise, for example with Thera-Bands (synthetic rubber bands used in exercising), do you breathe in through your nose when pulling the band out and blowing out through your mouth when pulling band together? Is this correct and where can I find more information on this? KC Klinger, RRT A. Dear KC, Textbooks on pulmonary rehabilitation can help you. I suggest one of Hodgkin and Connor's editions. Pursed lips breathing involves exhaling slowly against the lips that are partly closed as in whistling.
Dr. Tom
Increased Mucus and Shortness of Breath Since Medication Change I am tempted to get off the Spiriva and go back on Atrovent but with more doses of Atrovent. What would you recommend? Could the shortness of breath be related to the Spiriva? One of the possible side effects listed for Spiriva is difficulty breathing. Leo A. Dear Leo, Spiriva and Atrovent work through essentially the same mechanism. If you were better with Atrovent, I suggest returning to it, and taking it three or four times a day. Dr. Tom
“Breath Building” Devises for People with Emphysema Dot A. Dear Dot, I do not know about this device. It is probably an unnecessary gadget. I suggest normal walking and pursed lips breathing (see graphic above). Dr. Tom
What Happens if Bullae are not Surgically Removed? Jeff A. Dear Jeff, They will remain the same. There are some new valves under study that aim to reduce the volume of these bullae, but these studies are only done in major medical centers. Dr. Tom
Son had Multiple Lung Problems and Mom is Concerned about Pain and Tenderness around Chest Tube Wound Just recently he started complaining that he has pain and tenderness right around the site of the old chest tube wound (chest tube is a surgical inserted hollow, flexible drainage tube that is placed between the ribs and into the space between the inner lining and the outer lining of the lung, the pleural space, in order to drain blood, fluid, or air and allow full expansion of the lung). It feels somewhat sucken in around the site. He says it feels like a bruise and it is very tender to touch. Since the accident I tend to be a little hyper about him but should I make him see someone about this? He is 20 and thinks mom is a bit nutty about taking care of him. Beverly A. Dear Beverly, It is hard for me to tell what this is by the description. Since the accident is that far in the past, I suggest you do have him see his surgeon or a pulmonologist to determine the cause. Don’t apologize for being a caring mom. You both have been through a lot, and a sense of some anxiety is normal. Dr. Tom
Want to Understand Pulmonary Function Test (PFT) Results The results of my PFT were:
The fire dept. asked that everything be at 80%. I was an athlete all my life and never had asthma. I’m concerned because I really want the job but I can’t seem to breathe the out (exhale) all of the air that I breathe in (inhale) and the doctor said that I might have a mild obstruction in my lungs, but said that my lungs where in good shape. Please help me understand. Anthony A. Dear Anthony, The only numbers that have clinical meaning are the FVC and FEV1. You are close to normal. I do not think you have anything to be concerned about. Dr. Tom
Could the Medication for My Heart Condition cause Shortness of Breath? Question- I am on Amiodarone for Atrial Fibrillation (abnormal rhythm of the heart) and I'm experiencing all bad identifiable effects such as shortness of breath, severe gastric reflux, tremors and now atelectasis. Should I pursue this lung problem as a possible effect from the Amadarone? William A. Dear William, Yes. Amiodarone can cause serious lung reactions. Better get lung function tests. Dr. Tom
Are There any Medications that I Should Not Take Before a PFT? William A. Dear William, Stopping these drugs just before the pulmonary function tests, presumably spirometry, will not effect the results. Why are you taking such a high dose of prednisone? Dr. Tom
Lung Problems After Multiple Rounds of Drugs The only diagnosis I have been given is bronchitis. I have had 3 rounds of different antibiotic, 4 rounds of Prednisone and none of it has helped. The doctor even said he was confused with this. It just will not get any better - suggestions? Sharon A. Dear Sharon, Get a doctor to do spirometry to test your lung function. Chest x-rays and CT Scans do not tell how well your lungs are functioning. Your doctor should know this. Dr. Tom |
||||||||||
| 2025 American Association for Respiratory Care | ||||||||||