|
||||||||

Archive: Dr. Tom 44 Feel an Increasing Need for Oxygen My question is this. As my oxygen flow appears to need more assistance, I am concerned as to where this might be leading. Any comment would be appreciated. Bob A. Dear Bob, Increasing the liter flow, is not often the solution to shortness of breath. Shortness of breath comes from the work you have to do to breathe. This is greatly increased in COPD. Very few patients with COPD have an objective, that is a measured oxygen need by oximetry (a test that measures your oxygenation by using a machine called an oximeter) for those using oxygen for more than 4 liters. Better see your pulmonologist about this and have pulse oximetry done while you do various exercises. Keep active! Dr. Tom
Lung Problems Greta A. Dear Greta, Pleural thickening is usually a scar from an old infection. Antibiotics will not help this. Did your doctor measure the oxygen in your blood? If not, he is just guessing. Dr. Tom
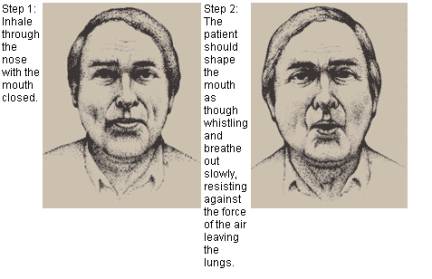
How Can I Improve My Oxygen Saturation? Dave A. Dear Dave, Your oxygen levels are quite low. Maybe you have interstitial fibrosis, and not COPD. The feeling of shortness of breath and your oxygen levels can be helped by “pursed lip breathing”; it will slow down the number of breaths you take and allows each breath to do more good for you. Steps to Pursed Lip Breathing
Dr. Tom Source of pictures:
Side Effects of Prednisone on Skin It starts with a bump that looks a lot like a mosquito bite, but it doesn't itch, it hurts and is warm to the touch. Sometimes these bumps get about as big as the size of a nickel and sometimes it is about as big as the size of 3 quarters put together. About a week later it goes down and sometimes forms a blister with this nasty white discharge. After it is completely down it leaves an ugly black mark. I have been getting these bumps for over a year now. My doctor tested me for diabetes but the results showed that I am not diabetic. She referred me to a dermatologist who told me that this was a side effect to steroids, but the strange thing is, they only form on the front and side part of my legs and thighs. Do you think that Prednisone could be the cause of this, and do you know if the effects are permanent? I am disturbed by the appearance but I am more concerned because I haven't heard too much about this condition. I never wear skirts or shorts anymore! Sonya A. Dear Sonya, This is not from prednisone. Consult a different dermatologist. Dr. Tom
Emergency Room Guidelines for CPAP and Bi-Pap The more technical stuff than what I seem to find when doing searches is what I need. Something for more in the acute ER setting and not home CPAP/Bi-Papa or OSA (Obstructive Sleep Apnea) therapies. Thanks. Beth A. Dear Beth, There are lots of articles in various journals about BI PAP used for non-invasive ventilation. Also on CPAP, which does not help ventilation, much, but has other beneficial effects on respiration. Consult the published literature. Dr. Tom
Bothered by “Smoker’s Cough” yet Never Smoked I was diagnosed with asthma in my 20's after a scuba-diving accident (don't ask). I only wheeze occasionally, and have tried to keep taking Atrovent and Pulmicort regularly. I have also been jogging regularly for the past 20 years (I am not very fast.) My question is: how come I still have this embarrassing “smoker's cough?” My spirometry FEV1 is usually normal, but my FEV1/FVC is usually around 70%. Second question: Is my smoker's cough going to turn into something worse, like COPD or emphysema. Penny A. Dear Penny, This is not a smoker’s cough, since you have never smoked. It will not lead to emphysema. Of course you could have a smoker's cough if you are exposed to environmental tobacco smoke, such as in bars or restaurants, or other places. But you need a diagnosis. Could be mild asthma. Consult a pulmonologist. Dr. Tom
Adair’s Benefits and Side Effects Many of the most recent asthma patients have stated that since they have been using “Advair” their symptoms have greatly decreased and life styles have improved. Physicians state less emergency room visits for asthma. I read recently about some bad side effects for using “Advair.” What is your opinion about this? Patricia A. Dear Patricia, Advair is very helpful in the maintenance management of asthma. Side effects in the long term are due to the corticosteroid component, flutacisone. These may include cataracts, diabetes and skin changes. Even osteopenia (a decrease in the amount of calcium and phosphorus in the bones), but these side effects are not common. Dr. Tom
Can Drugs cause Lung Problems? Several months ago my wife started having a hard time breathing. She quit smoking immediately and went to pulmonologist, believing she had advanced COPD. Her PFT's were all normal and her pulmonologist says it is anxiety. She has been on methadone for 12 years prior to an addiction to Percodan and Hycodan for eight years. I have read that long-term use of methadone can cause lung problems. Can you please give us any information on this? She is currently de-toxing from the methadone. Anything at all you can tell us or please guide us. Mr. Travis A. Dear Mr. Travis, Methadone will not damage the lungs, if used in prescribed doses. She does not have COPD since here spirometry measurements are normal. Dr. Tom
Thick Phlegm Kim A. Dear Kim, It certainly requires a diagnosis. Consult a pulmonologist. Dr. Tom
Support Information for People Living with Tracheotomies Thanks! J.R. A. Dear J.R. I do not know of such a book, written for patients. Sorry. DR Tom You might want to try an Internet site called Aaron’s Tracheotomy. This site was started and is maintained by the Mother of a child (Aaron), who has a tracheotomy. The site is geared to children and their parents, however there is quite a bit of information that may be of help to your mother. Dr. Tom
Criteria for Post Bronchodilator Spirometry Brian A. Dear Brian, In general I agree. But I think that post bronchodilator tests are over rated. Quite a few patients do not show an improvement in airflow on testing with a single bronchodilator in the clinic or office. Later they may have a large effect if bronchodilators and sometimes, corticosteroids are prescribed. Just like blood pressure. You do not expect the antihypertensive to work in 20 minutes. Dr. Tom
Looking for Dr. Wendell Petty Bill A. Dear Bill, I have never heard of Dr. Wendell Petty. There are several other Dr. Pettys in Colorado, but no Wendell. Did you consult a directory? Dr. Tom
Her Patient is having a Hard Time Finding CPAP After she was set up at home with this same mask, she started having pain from keeping her dentures in. She couldn't wear this mask without them. We then tried to fit her with different masks all in which she felt weren't working. We tried the Petite comfort gel, Small Profile Lite, Breeze, Nasal Aire II, Respironics Full Face (Panic Attack), and the Swift. She is currently on the Swift, but unhappy. Do you have any suggestions about a different mask? It would have to be simple, easy to put on and adjust. She has limited mobility. Thank you for any suggestions, Amy Amy A. Dear Amy, You have tried all the masks that I know about. I admire your diligence. Sorry I do not have more suggestions. Dr. Tom
A Request to Review DVD I have recently upgraded "Smoke Brake" (change the name to match the theme) and would like for you to view it once again. Dr. Grunberg is our scientific consult among others that is transforming it into one of the best programs (and freely available). The DVD is now a 59-minute multi-media production. Steve A. Dear Steve, I would be happy to review your DVD. Send it to my office at 899 Logan, Suite 103, Denver, CO. 80203. Dr. Tom
Pseudomonas and COPD There is not much information about pseudomonas in COPD but there is a lot about pseudomonas in cystic fibrosis. Does chronic infection with pseudomonas in COPD follow the same path as in cystic fibrosis e.g. development of the mucoid form and then steady deterioration of the lungs? Thank you. Jennifer A. Dear Jennifer, In general this is correct. You may want to try the inhaled Tobramycin an antibiotic used in CF, known as Tobi. Dr. Tom
Bad Taste after using Spiriva Terri A. Dear Terri, Sorry, no. I have not heard of this side effect. Dr. Tom
Oxygen Saturation Targets at Rest and with Exertion My question is in regards to oximetry testing while ambulating COPD and fibrosis patients. What are good target values for each (resting and with exertion)? Also what adjustments should be made so far as the liter flow to maintain these numbers? Gerry A. Dear Gerry, Liter flows should be monitored by pulse oximetry. Target saturations for rest and exercise are 90%-94%. It is hard to accomplish this in some fibrosis patients. Saturations in the range of 80-85% are well tolerated unless there is marked tachycardia (the heart is beating faster than a normal rate) or respiratory distress. Dr. Tom
Worried about Mother’s COPD Diagnosis She has a terrible cough, and I managed to force her to get an X-ray. These are the results.
CT scan showed extensive emphysema right upper lobe, calcified pleural plaque. He said she has borderline bronchodilator response. Pre bronchodilator FEV1 was 1.83 (75%) compared to post bronchodilator 2.05(84%), denoting a 12% change in FEV1. He said that she is a small group of smokers that have a susceptible gene to developing emphysema, and said I probably have it too. How long can my mother live? Since she stopped smoking her cough is gone. I live in New Zealand, and want your advice please. I am trying to find out as much as I can. Can she expect to live longer than 10 years...or more? Your advice would be appreciated. Angie A. Dear Angie, Your mother's FEV1 is pretty good. She should live at least 10 years, since she has stopped smoking. This assumes no other disease is present. COPD does cluster in families. The Alpha One Antitrypsin Deficiency (additional information resources are listed below) is the only proven hereditary risk factor that can be identified by a simple blood test. Your doctor will know about this blood test. Dr. Tom For more information on Alpha One Antitrypsin Deficiency see, Alpha 1 Foundation and/or Alpha 1 Net.
Peak Flow Meter Measurements Alzahrani A. Dear Alzahrani, Take the top one. Peak flow is just that, i.e. the airflow at the instant of maximum flow. It varies with effort. Dr. Tom
|
||||||||||
| 2025 American Association for Respiratory Care | ||||||||||