 |
|||||
|
|
Summer 2008 Improve Asthma Control by Knowing Your Triggers All Nebulizer Medications are NOT Created Equally News Bits
|
|
|
Asthmatics Are Still Going Without Controller Medications According to Ohio State University researchers who examined data from more than 800 million asthma-related visits to doctors’ offices between 1998 and 2004, asthma patients overall had 3.3 times higher odds of being prescribed controller medications in 2002 than in 1998. But use of these medications went on the decline beginning in 2003. The authors speculate negative reports about heart risks related to long-acting beta agonists might be partly to blame. The research also showed patients over age 65 had 54% lower odds of receiving a controller medication than patients between the ages of 35 and 64. Patients listed in the “other” race category in the survey, who were potentially of Asian or Hispanic background, were only 40% as likely to receive controller medications as white patients. However, no such disparities were seen when prescriptions for African-American and white patients were compared. The research appeared in the March issue of the Annals of Allergy, Asthma and Immunology. Researchers Link Gene Variants to Asthma The University of Chicago study was built on previous research that identified the gene variants in 700 members of an isolated and closely related religious community in South Dakota known as the Hutterites. In the new study, investigators confirmed the connection between the gene and the YKL-40 protein in three additional and more genetically diverse white groups in Chicago, Wisconsin, and Freiburg, Germany. “YKL-40 appears to serve as a marker for genetic susceptibility to asthma and decline in lung function,” James P. Kiley, PhD, director of the NHLBI division of lung diseases, was quoted as saying. “These findings will help pave the way for more research on pre-empting the development of disease.” The study appeared in the April 17 edition of the New England Journal of Medicine. New understanding for asthma and COPD Missouri researchers are working on a new way to diagnose, track, and possibly even treat asthma and COPD. In a study conducted in mice, investigators from Washington University School of Medicine in St. Louis found a common viral infection of the lung can leave behind a persistent trace that likely serves as an ongoing stimulus for a chronic immune response in the lung passages. The main culprit in this process is the inflammatory marker interleukin-13 (IL-13), which is normally activated for only short periods of time but can also be persistently activated after viral infection. The investigators discovered the specific immune pathway involved, finding that under these conditions, the pathway is set up to amplify its own activity. The combination of persistent activity and positive feedback leads to the long-term production of IL-13 as well as other substances that cause continuous inflammation in the lung tissue and the development of chronic lung disease. The researchers then detected this immune response in the lungs of people with severe asthma and COPD, finding that it produces a specific array of compounds that can be detected in the lung — and likely in the blood too — and may serve as diagnostic markers of disease. Now they are working to confirm their findings and believe if results prove positive, these markers could not only dramatically improve the diagnosis and monitoring of asthma and COPD, but also lead to treatments that target the underlying cause of the inflammatory process in individual patients. The study, which appeared in the May 18 issue of Nature Medicine, builds on previous work from the same group that uncovered another immune pathway that develops following respiratory viral infection and can lead to inflammatory lung disease. Asthma and suicide: A real risk
The study is based on data collected from 5,692 people age 18 and older who were included in the National Comorbidity Survey Replication. About 12% of the sample had asthma. Results associated asthma with suicidal attempts, but not with suicidal thoughts that didn’t lead to an actual attempt. Female gender, current smoking, alcoholism, nicotine addiction, and depression/anxiety upped the risk, but the findings held true even after researchers adjusted for concurrent mental health conditions and sociodemographic factors. The authors write, “More research is needed to further elucidate the mechanism of the remaining association between asthma and suicide attempts. Modification of smoking behaviors and effective treatment of depression, anxiety, alcohol abuse, and possibly asthma are important suicide prevention strategies.” |
|

 Too many asthma patients are still not receiving controller medications, despite the fact that the national asthma guidelines have been recommending these medications since they were first released in 1997.
Too many asthma patients are still not receiving controller medications, despite the fact that the national asthma guidelines have been recommending these medications since they were first released in 1997.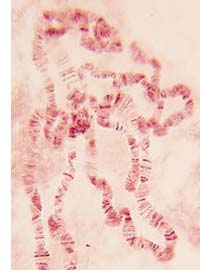 New research sponsored by the National Heart, Lung, and Blood Institute (NHLBI) suggests asthma risk is related to variations in a gene called CHI3L1; and measuring blood levels of a protein known as YKL-40, which is regulated by the gene and known to be elevated in people with asthma, could be a good way to assess for susceptibility to the condition. In the study, people with one type of genetic variation had higher levels of YKL-40, while those with another variation had lower levels and a lower risk of developing asthma.
New research sponsored by the National Heart, Lung, and Blood Institute (NHLBI) suggests asthma risk is related to variations in a gene called CHI3L1; and measuring blood levels of a protein known as YKL-40, which is regulated by the gene and known to be elevated in people with asthma, could be a good way to assess for susceptibility to the condition. In the study, people with one type of genetic variation had higher levels of YKL-40, while those with another variation had lower levels and a lower risk of developing asthma. Many studies have examined the link between asthma and psychological distress. Now researchers publishing in the May issue of the Annals of Allergy, Asthma & Immunology report new evidence that asthma may actually put people at higher risk for suicide as well.
Many studies have examined the link between asthma and psychological distress. Now researchers publishing in the May issue of the Annals of Allergy, Asthma & Immunology report new evidence that asthma may actually put people at higher risk for suicide as well.